How Prior Authorization Punishes the Sickest Patients
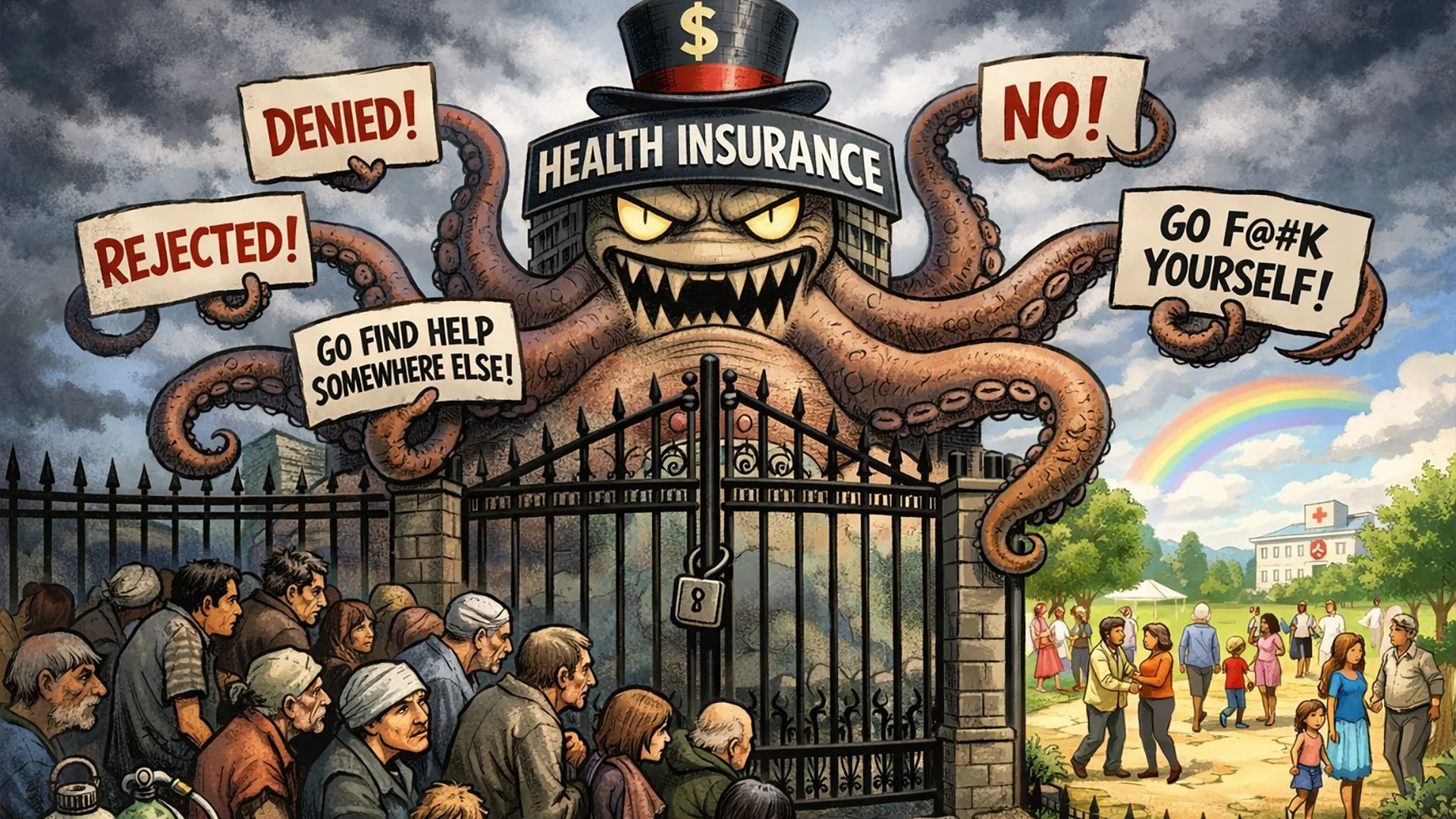
They keep calling it reform. Patients experience something else entirely.
I want to start with a woman who did everything she was told to do. Her name is Sheldon Ekirch. She lives in Virginia and pays more than $600 a month for health insurance. In 2023, she began experiencing numbness and burning throughout her body. Doctors eventually diagnosed her with small fiber neuropathy. Multiple specialists, including neurologists at the University of Virginia and Virginia Commonwealth University, reviewed her case and agreed on a treatment plan. IVIG. The recommendation was not casual. It followed symptoms, testing, and expert consensus. Anthem denied it anyway.
After appeals. After documentation. After time passed and her condition worsened. Anthem issued a final denial. Then something revealing happened. An Anthem employee, a nurse advocate, suggested Ekirch contact the drug manufacturer directly and ask about charity programs. Her insurer collected premiums, reviewed the case, rejected the treatment, and redirected responsibility elsewhere. Not because the treatment posed danger. Not because it lacked any medical basis. Because it did not meet Anthem’s internal criteria for effectiveness. That moment captures the reality of prior authorization better than any policy memo.
I was quoted recently in a KFF Health News investigation into prior authorization that documented case after case of sick patients facing denials despite years of promised reform. The article included physicians, economists, policy experts, and people living inside the system’s delays. I said something simple and uncomfortable. Patients are finally realizing they are not alone. For years, people internalized these experiences as personal failure or bad luck. Now they recognize pattern.
For decades, insurers have framed prior authorization as a safeguard. They say it reduces waste, prevents unnecessary care, and protects patients from harm. Those claims sound reasonable until you examine who gets caught and when. Prior authorization disproportionately targets people who need expensive care. Advanced imaging. Chemotherapy. Infusions. Inpatient admissions. It shows up when stakes are highest and time carries consequence. The rules vary by insurer and plan, and the data remains largely opaque. Transparency requirements exist but enforcement remains weak. Even experts struggle to quantify impact because insurers do not publish comprehensive information. What we do know comes from lived experience.
In 2023, a man diagnosed with follicular lymphoma needed a whole body PET scan to stage his disease. His oncologist ordered it. EviCore, a subsidiary of Cigna that handles prior authorization decisions, denied the request. The patient’s son is an internal medicine physician. He spent hours on the phone arguing that current medical guidelines supported the scan. Eventually, approval came through. But weeks passed. Appointments were scheduled and canceled. The family waited, unsure whether the cancer was spreading. Cigna later said the denial resulted from incomplete clinical information and promised improvements to submission processes. That explanation may be technically accurate and morally irrelevant. If a family with a physician cannot navigate this system without delay, everyone else faces worse odds.
This is where insurers pivot to optics. Over the past several years, companies have announced improvements to prior authorization. Faster timelines. Electronic submissions. Gold card programs that exempt certain physicians with high approval rates. Executives speak about simplification and efficiency. One healthcare executive who reviewed these changes closely described them as almost a public relations stunt. When examined in detail, the services most frequently denied remain untouched. That gap fuels frustration and distrust.
In January, a breast reconstruction surgeon in Austin, Texas, posted a video describing how UnitedHealthcare questioned whether her breast cancer patient needed inpatient admission on the day of surgery. The video spread quickly. Millions watched. UnitedHealthcare responded by hiring lawyers and demanding a correction and apology. The facts remain disputed. The reaction speaks clearly. For years, patients and physicians have used public pressure to force approvals. What changed recently is scale. Stories began to sound identical across insurers, diagnoses, and regions. People stopped asking what they did wrong and started asking why this keeps happening.
That is the shift I described as unified anger.
I know something about systems that claim to protect while causing harm. At 21, I survived brain cancer. I received craniospinal radiation over 33 days. More than 5,000 rads. That experience stripped away illusions about institutional benevolence. It taught me how easily people disappear behind policy language. It taught me that survival often requires resistance rather than compliance. Prior authorization operates on the same fault line.
Insurers insist prior authorization affects a small percentage of claims. UnitedHealthcare says fewer than 2 percent require it and that 99 percent are approved quickly. Those statistics flatten reality. They erase concentration of harm. Medicare Advantage enrollees encounter prior authorization far more often than those in traditional Medicare. High cost services trigger it most frequently. Chemotherapy. Skilled nursing. Hospital stays. These are not edge cases. These are moments of vulnerability.
Insurers sometimes cite examples where prior authorization caught an error. A wrong sided surgery. An incorrect dosage. Those examples make convenient talking points. They do not justify a system that routinely delays appropriate care for thousands of others.
IVIG sits at the center of this tension. It is not a miracle drug. Evidence varies by condition. Some studies show benefit. Others show limited effect. That uncertainty becomes leverage. For patients like Ekirch, uncertainty translates into suffering. She watches peers advance in careers and families while she struggles to function. She pays premiums. She follows rules. She appeals decisions. She gets told to ask a pharmaceutical company for charity.
When insurers talk about reform, this is what it looks like in practice.
Politicians continue to announce bipartisan efforts to fix prior authorization. Bills mandate electronic systems. Timelines shorten. Gold card programs expand. Some lawmakers call for abolition. None of this changes the underlying incentive. As long as insurers remain accountable to shareholders, denial remains a tool and delay remains strategy. Administrative burden shifts cost outward. Advocates describe reform as Whac A Mole. Patients live in the gaps.
Ekirkh’s last hope rests with a state insurance bureau that occasionally overturns denials. She waits. She manages expectations. She braces for disappointment. That waiting carries a toll no spreadsheet captures. Lost time. Lost income. Deteriorating health. Psychological exhaustion. Families stretched thin. Physicians burned out. Trust eroded.
This is not accidental. It is design.
What changed is recognition. Patients stopped personalizing blame. They compared notes. They named the pattern. Unified anger does not guarantee policy change, but it guarantees scrutiny. It invites journalists, regulators, and lawmakers who sense pressure. That recognition carries risk for insurers who rely on silence and fragmentation.
I do not write this to inspire. I write it to document. If you are navigating prior authorization, your experience fits a pattern. If you are a caregiver watching delays compound, your frustration aligns with others. If you are a clinician spending hours on hold, your exhaustion has context.
Here is the action. Document denials. Save letters. Record timelines. Share stories publicly when safe. File complaints with state regulators. Support reporting that exposes pattern. Refuse to internalize blame. Silence protects the system. Pattern recognition weakens it. Pressure accumulates. Scrutiny intensifies. The cost of denial rises.
I survived something that taught me institutions change only when exposure becomes unavoidable. Prior authorization thrives on fragmentation. That era is ending. And the people who benefit from it know exactly why.